By: Amanda Gordon, RD, LDN, IBCLC and Dan Frazier, RDN-AP, CNSC
Parents feel fulfilled when they feed their children healthy foods. Foods that are fresh, colorful and taste good. Foods sourced from quality ingredients. Food that are less processed and contain fiber and other nutrients that make our bodies work well. Foods that provide energy.
There is an important movement afloat in the nutrition world and a growing body of scientific evidence that supports the idea that children with feeding tubes should eat real food too. Tasty, nutrient-dense, colorful food. The same food that their parents eat. The same food that other children eat.
February 10-14 is Feeding Tube Awareness Week, a campaign initiated by the Feeding Tube Awareness Foundation to bring awareness about tube feeding (https://www.feedingtubeawareness.org/). So, what better time than now to talk and think about children with feeding tubes.
Many adults and children alike are reliant on tube feedings at home to deliver adequate nutrition and hydration. Studies using Medicare and Medicaid data in the United States indicate that the use of home tube feeding is on the rise in the United States.1 According to data from the Feeding Tube Awareness Foundation, children 18 and under represent about 40% of the tube fed population.1 There are many reasons why a child may have a tube placed for feeding and hydration. These can include medical diagnoses, including prematurity, physical, anatomical, or neurologic conditions.
Feeding tubes can also be placed for children with swallowing difficulties and in situations of pediatric feeding disorders (which are also on the rise in the US).2 And, for those who may question or doubt the reality of a pediatric feeding disorder being a real thing, just ask any family who has had a feeding tube placed in their child for this reason.
Feeding children through a feeding tube can be very stressful for families. It can take the whole concept of eating and turn it into something medical. Eating is supposed to be social and enjoyable. When nutrition has to be delivered through a tube, this can change the dynamics, meal times, and how a family views nutrition for their child. And for good reason. Up until a few years ago, most children in the US were fed primarily medical formulas and nutrition supplements through a feeding pump that delivered nutrients on a set regimen over a 24 hour period. (No wonder this would feel more medical that nourishing).
However, families today have more options for feeding children with tubes who are over 12 months old. There is a strong movement, backed by growing scientific research, to feed real food to children with feeding tubes. Yep. Chicken, fish, eggs, fruits, vegetables, milk, yogurt and other dairy. All kinds of stuff.
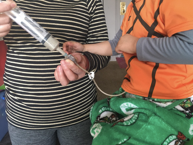
While some children have medical conditions that require specialized formulas to deliver specific nutrients through a feeding tube, many families are moving away from conventional formulas as possible. With the help of Registered Dietitians who specialize in this area, children with feeding tubes now have the opportunity to eat the same foods that their families, caregivers, and friends eat. Parents blending foods in their kitchens are able to feed this to their children. Recipe sharing and books are now published on feeding table foods to children with feeding tubes. There are also a growing number of companies that are creating wholesome meals meant for children with feeding tubes.
Feeding children real foods, table foods or family foods can help children feel better. Studies indicate that children who eat food by tube instead of formula often have improved tube feeding tolerance due to an improvement in gastrointestinal symptoms such as nausea, vomiting, diarrhea, and gagging/retching3,4,5. Additionally, for kiddos able to eat orally, studies indicate that those using real food versus formula have decreased oral aversion and increased oral intake4.
Parents and caregivers often feel better as well. They feel more empowered by the ability to nourish their children well. Many families relish the opportunity to feed their children family and culturally-appropriate foods. Most importantly, they often feel less stress overall as the feeding experience normalizes in a sense and doesn’t alienate their child. Not surprisingly, parents using blenderized tube feeding reported feeling that their child was happier and healthier; they also unanimously recommended blenderized tube feeding to other parents6.
In many ways, the discussion around feeding real food feels full circle. Prior to the inception of formula in the 1960s, people with feeding tubes were given real food. It is exciting to see this become popular again and given the clinical studies substantiating this practice, in conjunction with the overwhelmingly positive response from parents, feeding real food to children with feeding tubes will likely become more common.
The USDA Dietary Guidelines recommend eating a variety of nutrient dense foods for all Americans. Children with feeding tubes should not be excluded from the opportunity to enjoy real food. It is our hope that families and Registered Dietitians continue to advocate for the concept of feeding as eating, not a medical procedure.
Amanda Gordon, RD, LDN, IBCLC is a pediatric dietitian at Feed to Succeed, LLC, a private pediatric nutrition practice. Feed to Succeed works with families on food-based tube feeding diets for children and on weaning children from tube feedings. For more information, visit https://feedtosucceed.com
Dan Frazier, RDN-AP, CNSC is a Registered Dietitian with Real Food Blends. Real Food Blends makes 100% real food meals for individuals with feeding tubes. To learn more, visit http://www.realfoodblends.com
1. Mundi MS, Pattinson A, McMahon MT, Davidson J, Hurt RT. Prevalence of Home Parenteral and Enteral Nutrition in the United States. Nutr Clin Pract. 2017;32(6):799-805. doi:10.1177/0884533617718472
2. Forbes D, Grover Z. Tube feeding: Stopping more difficult than starting. J Paediatr Child Health. 2015;51(3):245-247. doi:10.1111/jpc.12763
3. Hron, B., Fishman, E., Lurie, M., Clarke, T., Chin, Z., Hester, L., Burch, E. and Rosen, R. (2019). Health Outcomes and Quality of Life Indices of Children Receiving Blenderized Feeds via Enteral Tube. The Journal of Pediatrics, 211, pp.139-145.e1.
4. Pentiuk, S., O’Flaherty, T., Santoro, K., Willging, P. and Kaul, A. (2011). Pureed by Gastrostomy Tube Diet Improves Gagging and Retching in Children With Fundoplication. Journal of Parenteral and Enteral Nutrition, 35(3), pp.375-379.
5. Batsis, I., Davis, L., Prichett, L., Wu, L., Shores, D., Au Yeung, K. and Oliva- Hemker, M. (2019). Efficacy and Tolerance of Blended Diets in Children Receiving Gastrostomy Feeds. Nutrition in Clinical Practice.
6. Gallagher, K., Flint, A., Mouzaki, M., Carpenter, A., Haliburton, B., Bannister, L., Norgrove, H., Hoffman, L., Mack, D., Stintzi, A. and Marcon, M. (2018). Blenderized Enteral Nutrition Diet Study: Feasibility, Clinical, and Microbiome Outcomes of Providing Blenderized Feeds Through a Gastric Tube in a Medically Complex Pediatric Population. Journal of Parenteral and Enteral Nutrition, 42(6), pp.1046-1060.